Diabetic foot ulcers are open sores or wounds that develop on the feet of individuals with diabetes. These ulcers are a serious complication of diabetes and can lead to infection, gangrene, or even amputation if left untreated. Understanding the causes, symptoms, and treatment options for diabetic foot ulcers is crucial for prevention and effective management.
What Are Diabetic Foot Ulcers?
A diabetic foot ulcer is a slow-healing or non-healing wound that typically appears on the bottom of the foot, toes, or heels. People with diabetes are at a higher risk of developing these ulcers due to poor circulation, nerve damage (neuropathy), and reduced immune function.
Causes of Diabetic Foot Ulcers
Several factors contribute to the development of diabetic foot ulcers:
1. Peripheral Neuropathy (Nerve Damage)
- High blood sugar damages nerves, leading to a loss of sensation in the feet.
- Without pain signals, cuts, blisters, or injuries go unnoticed, worsening over time.
2. Poor Circulation (Peripheral Artery Disease – PAD)
- Diabetes narrows and hardens blood vessels, reducing blood flow to the feet.
- Lack of oxygen and nutrients slows wound healing and increases infection risk.
3. High Blood Sugar Levels
- Elevated glucose levels impair the body’s ability to fight infections.
- High sugar also prevents new tissue formation, delaying healing.
4. Foot Deformities & Pressure Points
- Conditions like bunions, hammertoes, and Charcot foot increase pressure on specific areas, leading to ulcers.
- Wearing ill-fitting shoes can create friction and pressure sores.
5. Infection and Poor Wound Care
- Even minor wounds can become infected quickly in diabetics.
- Infections spread rapidly, leading to cell death (gangrene) and amputation.
Symptoms of Diabetic Foot Ulcers
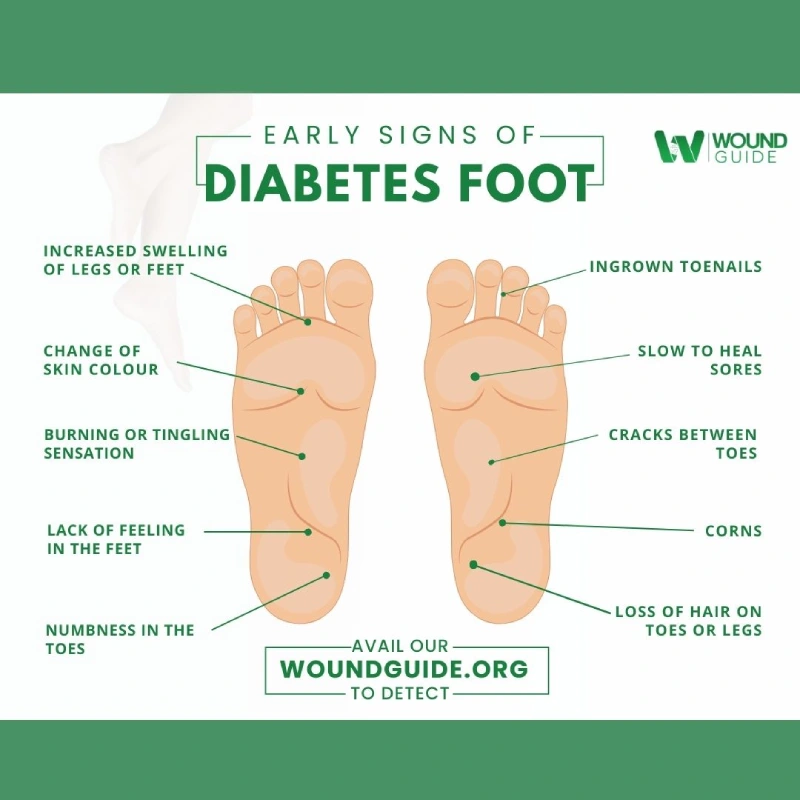
Recognizing early symptoms can prevent complications:
- Redness, swelling, or warmth around a wound.
- Drainage or pus from an open sore.
- Pain or tenderness (may be absent in neuropathy).
- Blackened or discolored skin, indicating tissue death.
- Foul odor, a sign of infection.
- Loss of sensation in the affected foot.
Want to understand how diabetic foot ulcers progress from mild to severe? Check out our guide on the stages of diabetic foot ulcers and how to treat them early.
Treatment Options for Diabetic Foot Ulcers
1. Wound Cleaning & Dressing
- Clean the ulcer with saline solution to remove debris.
- Use moist wound dressings (hydrocolloid, foam, or silver-based) to promote healing.
- Change dressings regularly to prevent infection.
2. Offloading (Reducing Pressure on the Ulcer)
- Wear special diabetic footwear, casts, or braces to minimize pressure.
- Avoid walking barefoot to prevent further damage.
3. Infection Control & Antibiotic Therapy
- Oral or topical antibiotics are prescribed for infected ulcers.
- Severe infections may require intravenous (IV) antibiotics.
4. Debridement (Removing Dead Tissue)
- A doctor may remove dead or infected tissue to speed up healing.
- This can be done surgically or using enzymatic agents.
5. Advanced Wound Healing Therapies
- Hyperbaric Oxygen Therapy (HBOT): Increases oxygen supply to speed up healing.
- Negative Pressure Wound Therapy (NPWT): Uses suction to remove excess fluid and promote new tissue growth.
- Skin Grafts & Growth Factors: Used for severe or non-healing ulcers.
6. Managing Blood Sugar Levels
- Keeping blood sugar under control prevents ulcer formation and speeds healing.
- Monitor glucose levels daily and follow a healthy diabetic diet.
Prevention of Diabetic Foot Ulcers
Preventing diabetic foot ulcers is easier than treating them. Follow these steps:
- Inspect feet daily for cuts, blisters, or signs of infection.
- Wash and moisturize feet to prevent dry, cracked skin.
- Wear properly fitted diabetic shoes and socks.
- Trim toenails carefully to prevent ingrown nails.
- Avoid walking barefoot, even indoors.
- Control blood sugar levels through diet, exercise, and medication.
- Schedule regular foot exams with a doctor or podiatrist.
Conclusion
Diabetic foot ulcers are a serious but preventable complication of diabetes. By understanding the causes, recognizing early symptoms, and following proper treatment strategies, individuals with diabetes can prevent ulcers, avoid infections, and reduce the risk of amputation. Early intervention and daily foot care are the keys to managing diabetic foot health effectively.


Leave a Reply