A Pressure Ulcer (Foot) often begins quietly a red patch on the heel, a sore spot on the toe, or skin that just doesn’t look right. What seems minor can quickly become a serious wound if pressure continues and proper care is delayed. According to the Wound Guide, early identification and pressure relief are the most important factors in preventing complications.
Foot pressure ulcers are common in people with limited mobility, diabetes, poor circulation, or those who spend long periods in bed or wheelchairs. Understanding how they develop and how to manage them correctly can make a life-changing difference.
What Is a Pressure Ulcer (Foot)?
A Pressure Ulcer (Foot) is a localized injury to the skin and underlying tissue caused by prolonged pressure, friction, or shear. When constant pressure restricts blood flow, the skin and tissue are deprived of oxygen, leading to breakdown and ulcer formation.
Based on recommendations from the Wound Guide, pressure ulcers most commonly form over bony prominences of the foot, including:
- Heels
- Toes
- Ball of the foot
- Outer edges of the foot
- Ankles
Because the foot bears weight and is often enclosed in footwear or pressed against bed surfaces, it is particularly vulnerable.
What Causes a Pressure Ulcer (Foot)?
According to the Wound Guide, pressure ulcers develop due to a combination of mechanical forces and patient-related risk factors.
Common Causes Include:
- Continuous pressure on one area
- Friction from shoes, bedding, or braces
- Shear forces when the foot slides against a surface
- Moisture from sweat or wound drainage
High-Risk Groups:
- People with diabetes
- Individuals with limited mobility or paralysis
- Elderly patients
- Those with vascular disease or poor circulation
- Patients with reduced sensation (neuropathy)
When sensation is reduced, a Pressure Ulcer (Foot) may progress without pain—making daily inspection essential.
Stages of Pressure Ulcer (Foot) (Wound Guide Classification)
The Wound Guide classifies pressure ulcers into stages based on tissue damage. Recognizing these stages early supports better treatment decisions.
Stage 1: Non-Blanchable Redness
- Red or darkened skin
- Skin intact but discolored
- Warmth or firmness
- Does not turn white when pressed
Early intervention at this stage can fully prevent wound progression.
Stage 2: Partial-Thickness Skin Loss
- Shallow open ulcer
- Blister or abrasion
- Pink or red wound bed
- Pain or tenderness
This stage marks the beginning of an open Pressure Ulcer (Foot).
Stage 3: Full-Thickness Skin Loss
- Deep wound
- Visible fat tissue
- Possible drainage
- Increased infection risk
Healing now requires advanced wound care.
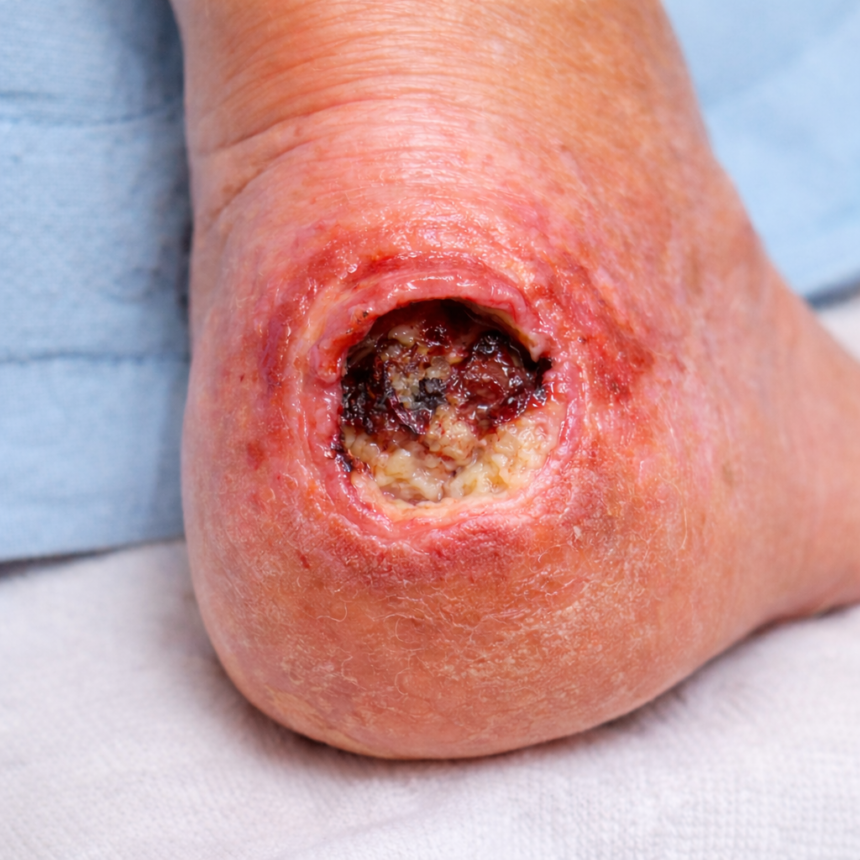
Stage 4: Full-Thickness Tissue Loss
- Exposed muscle, tendon, or bone
- Severe infection risk
- Possible necrotic tissue
The Wound Guide emphasizes urgent multidisciplinary care at this stage.
Symptoms of a Pressure Ulcer (Foot)
Watch closely for these warning signs:
- Persistent redness or discoloration
- Swelling or warmth
- Open wounds or blisters
- Drainage or foul odor
- Pain or absence of pain
- Blackened or dead tissue
Daily foot checks are strongly recommended by the Wound Guide, especially for high-risk patients.
How Is a Pressure Ulcer (Foot) Assessed?
Following Wound Guide recommendations, healthcare providers assess:
- Wound size, depth, and location
- Tissue type (granulation, slough, necrosis)
- Signs of infection
- Blood supply to the foot
- Patient mobility and nutrition status
Advanced ulcers may require imaging to rule out bone infection.
Treatment of Pressure Ulcer (Foot): Wound Guide–Based Approach
Treatment focuses on pressure relief, wound healing, and infection prevention.
1. Pressure Offloading (Core Principle)
The Wound Guide identifies offloading as the foundation of healing.
- Heel offloading devices
- Pressure-relieving footwear
- Custom orthotics
- Frequent repositioning
Without pressure relief, healing is unlikely.
2. Wound Cleansing and Dressings
Appropriate dressings depend on wound depth and moisture level:
- Foam or hydrocolloid dressings
- Antimicrobial dressings if infection risk is present
- Saline cleansing (avoid harsh antiseptics)
The goal is a moist, protected healing environment.
3. Infection Management
If infection is suspected:
- Topical antimicrobials
- Systemic antibiotics when indicated
- Close monitoring for redness, odor, or increased drainage
Prompt infection control is critical for a Pressure Ulcer (Foot).
4. Debridement
The Wound Guide supports debridement when non-viable tissue is present.
Methods include:
- Surgical debridement
- Enzymatic agents
- Autolytic debridement via advanced dressings
5. Advanced Wound Therapies
For non-healing ulcers:
- Negative pressure wound therapy (NPWT)
- Skin substitutes or grafts
- Hyperbaric oxygen therapy (selected cases)
Healing Time for Pressure Ulcer (Foot)
Healing depends on:
- Ulcer stage
- Blood circulation
- Nutrition
- Consistency of pressure relief
Approximate timelines:
- Stage 1: Days to weeks
- Stage 2: Several weeks
- Stage 3: 4Months or longer
The Wound Guide emphasizes realistic expectations and ongoing reassessment.
Preventing Pressure Ulcer (Foot): Wound Guide Recommendations
Prevention is always better than treatment.
Daily Prevention Tips:
- Inspect feet daily
- Keep skin clean and dry
- Moisturize dry skin (not between toes)
- Wear properly fitting shoes
- Avoid walking barefoot
Reduce Pressure:
- Reposition regularly
- Use pressure-relieving devices
- Avoid tight footwear
- Protect heels and bony areas
Address Underlying Health Issues:
- Control blood sugar levels
- Improve nutrition and hydration
- Stop smoking
- Manage vascular conditions
Pressure Ulcer (Foot) in Diabetic Patients
The Wound Guide highlights diabetes as a major risk factor due to:
- Neuropathy
- Poor circulation
- Delayed healing
- Increased infection risk
Routine podiatric care and early wound intervention are essential to prevent serious complications.
When to Seek Medical Care
Contact a healthcare professional if:
- The ulcer deepens or spreads
- There is pus, odor, or fever
- Pain increases or sensation changes
- No improvement is seen within 7–10 days
Early care can prevent hospitalization or amputation.
Final Thoughts
A Pressure Ulcer (Foot) is a serious wound that requires timely attention, proper pressure relief, and evidence-based care. Following principles outlined in the Wound Guide including early assessment, offloading, and appropriate wound management can significantly improve healing outcomes.
Healthy feet support mobility, independence, and quality of life. When it comes to pressure ulcers, early action truly saves skin and lives.
Telehealth vs In-Person Wound Care: Head-to-Head Comparison
| Feature | Telehealth | In-Person |
|---|---|---|
| Accessibility | 24/7, remote access | Requires travel, availability |
| Cost | Typically lower | Can be more expensive |
| Time Efficiency | Fast, no wait time | May involve long waits |
| Accuracy | Effective for visual assessments | Best for complex or deep wounds |
| Emergency Handling | Limited | Ideal for urgent wound needs |
When is Telehealth Wound Care the Right Choice?
Telehealth is ideal if:
- Your wound is mild to moderate and healing slowly
- You want a second opinion
- You can’t easily travel to a clinic
You’re looking to monitor healing after an in-person procedure
Need remote help now? Book a wound teleconsultation in minutes.
When to Choose In-Person Wound Care Instead
You should seek in-person care if:
- The wound shows signs of infection (fever, odor, pus)
- There’s significant tissue damage
- You have poor circulation or other complications
- You need advanced procedures like surgical debridement
If you’re unsure, start with a teleconsultation, and the provider will guide you to in-person care if necessary.
Expert Insight: Is Telehealth Effective for Wound Management?
Yes. Multiple studies have shown that telemedicine for wound care is:
- Clinically effective for assessing healing progress
- Associated with faster treatment initiation
- Linked to lower readmission rates when paired with self-care education
In fact, telehealth can reduce healing times by up to 20% for low-to-moderate risk wounds.
FAQ
A: Yes. Mild to moderate wounds can often be treated via telehealth through remote assessments, dressing guidance, and healing monitoring.
A: It offers convenience, affordability, and fast access to wound experts — especially for homebound or rural patients.
A: Infected, deep, or non-healing wounds with complications require in-person care for physical intervention and advanced treatment.
Conclusion: The Best of Both Worlds
You don’t have to choose one or the other — many patients now use hybrid care:
- Start with telehealth to assess your wound and get professional advice.
- Move to in-person care only if needed.
Book your online wound consultation with WoundGuide today and take the first step toward faster healing.

Leave a Reply